NSAIDs, Your Gut, and the Hidden Cost of Pain Relief
- Julien Boillat

- Jul 30, 2025
- 3 min read
Introduction: More Than Just Pain Relief
Non-steroidal anti-inflammatory drugs (NSAIDs or AINS in French), like ibuprofen, naproxen, and aspirin, are among the most commonly used medications for muscle aches, joint pain, and headaches. While effective at relieving pain and inflammation, frequent or chronic NSAID use comes with hidden consequences—particularly for your gut, liver, and long-term metabolic health. In this article, we’ll explore how these seemingly harmless pills may disrupt your body's internal balance and contribute to chronic inflammation.
Part 1: How NSAIDs Damage the Gut Barrier
The Gut Lining: Your First Line of Defense
The gut barrier is a one-cell-thick lining that separates your internal body from the trillions of microbes and foreign particles in your digestive tract. This barrier is held together by tight junctions that regulate what gets absorbed and what stays out. When healthy, it selectively allows nutrients into the bloodstream while keeping harmful substances like bacterial toxins out.
Prostaglandins: The Unsung Heroes
NSAIDs relieve pain by inhibiting enzymes called COX-1 and COX-2, which produce prostaglandins. While prostaglandins are involved in pain and inflammation, they also play a crucial role in protecting the gut:
Promoting mucus and bicarbonate secretion
Supporting blood flow to gut tissues
Aiding in cellular repair
When prostaglandin levels drop due to NSAIDs, the mucus layer thins, blood flow decreases, and the gut lining becomes fragile. This makes the barrier more permeable—a condition often referred to as "leaky gut."
Leaky Gut and Inflammation
A weakened gut barrier allows bacterial fragments—especially lipopolysaccharides (LPS)—to enter the bloodstream. These LPS molecules come from the outer membrane of Gram-negative bacteria that live in the gut. Once in circulation, they trigger the immune system, causing chronic low-grade inflammation. This has been linked to:
Insulin resistance
Fatty liver disease (NAFLD)
Brain fog and mood disturbances
Increased risk of cardiovascular disease
Part 2: How NSAIDs Alter the Microbiome
NSAIDs don’t just affect the gut lining—they also disrupt the gut microbiome, the complex ecosystem of bacteria living in your digestive tract. Chronic NSAID use:
Reduces beneficial species (like Bifidobacteria and Lactobacilli)
Encourages growth of harmful, LPS-producing bacteria
Reduces short-chain fatty acid (SCFA) production, which is essential for gut healing and anti-inflammatory effects
This imbalance (called dysbiosis) amplifies the problem: more LPS-producing bacteria, less healing capacity, and further compromise of the gut barrier.
Part 3: The Domino Effect – From Gut to Liver, Brain, and Metabolism
LPS, Inflammation, and Reactive Oxygen Species (ROS)
Once LPS enters circulation, it activates immune cells (via TLR4 receptors), triggering a release of inflammatory cytokines like IL-6 and TNF-alpha. It also leads to increased production of Reactive Oxygen Species (ROS) in the mitochondria.
ROS are natural byproducts of metabolism, but in excess they damage cells and organelles, fueling more inflammation—a vicious cycle.
The Liver's Burden
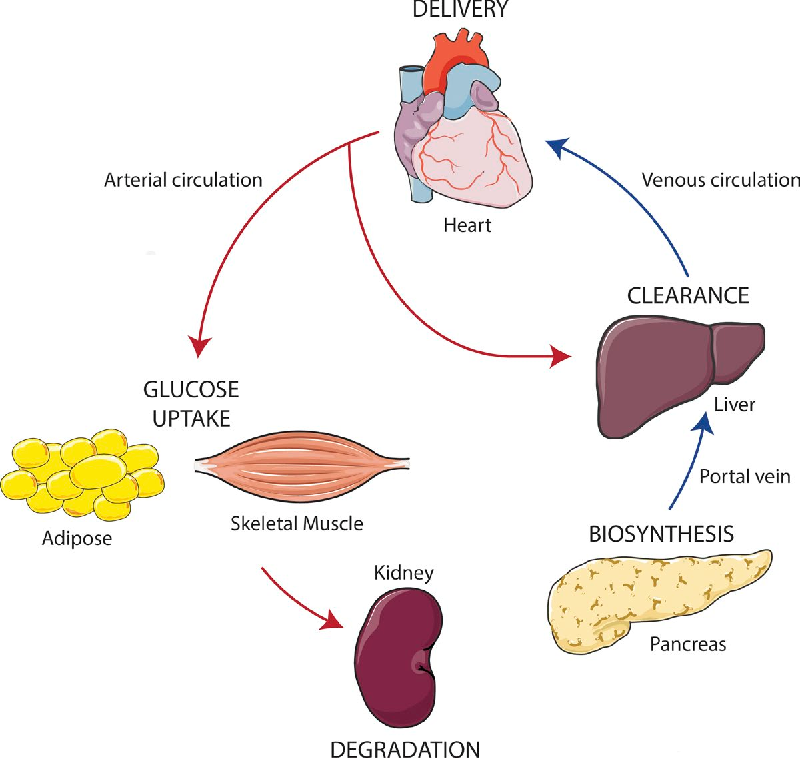
The liver is the first organ to receive blood from the gut via the portal vein. It tries to neutralize LPS using immune cells called Kupffer cells. But chronic exposure overwhelms the liver, contributing to:
Liver inflammation
Fat accumulation (steatosis)
Elevated liver enzymes (ALT, AST)
The Metabolic Consequences
This cascade—from gut leakiness to liver overload and systemic inflammation—ultimately disrupts glucose and fat metabolism. The result:
Insulin resistance
Increased fat storage (especially visceral fat)
Higher risk of metabolic syndrome and type 2 diabetes
Conclusion: Pain Relief Comes with a Price
While NSAIDs offer short-term relief, they can quietly set off long-term problems by weakening your gut barrier, disturbing your microbiome, and driving systemic inflammation. The next time you reach for a painkiller, remember that the cost may go far beyond your stomach—it could affect your entire metabolic health.
Practical Tips for Safer Use
Use NSAIDs only when necessary and avoid long-term use unless prescribed
Support your gut with a fiber-rich diet, fermented foods, and probiotics
Stay active and manage stress to protect gut integrity
If chronic pain persists, consider root-cause approaches like physiotherapy, anti-inflammatory nutrition, or lifestyle changes
Protect your gut—your entire health depends on it.




Comments